Eosinophilic esophagitis
Eosinophilic esophagitis (EoE) is a rare, chronic disease, but it is increasingly diagnosed both in adults and children.
Common symptoms include:
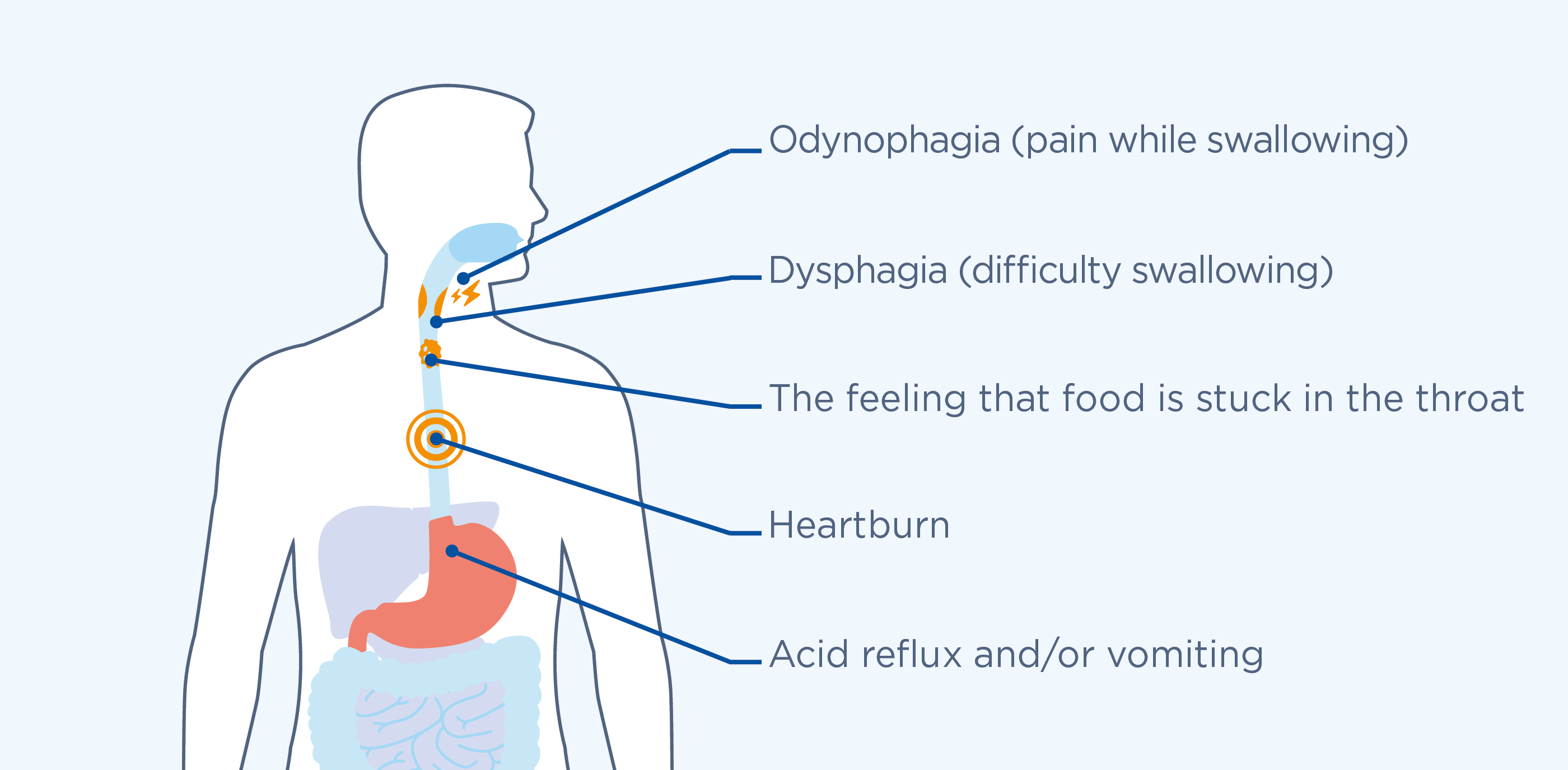
The frequency of the symptoms can vary, depending on the age of the individual: in adults the most common symptoms are difficulty swallowing, food getting stuck in the esophagus, stomach pain and acid reflux; whereas, in children acid reflux and/or vomiting, stomach and abdominal pain have been observed.
EoE is believed to be a form of allergic reaction, this means it can easily be triggered by allergens - substances in the environment, particularly in foods, that can cause an allergic reaction in susceptible individuals. This autoimmune response can cause constant inflammation of the esophagus, which prevents the organ from carrying out its normal function of transporting food from the mouth to the stomach. The condition is also believed to be hereditary, which makes certain people more naturally predisposed to developing the disease.
Diagnosis of EoE must be carried out by a specialist doctor and involves:
- Clinical characteristics: identification of the esophageal symptoms associated with the disease;
- Endoscopic evidence: identification of anomalies of the esophagus by an endoscopy, which is carried out using a small tube equipped with a tiny video camera that is guided down the throat until it reaches the esophagus to visualise the inside of the organ. This allows for the identification of any inflammation or alterations to the tissue;
- Histological evidence: taking biopsies, i.e. collecting and analysing small tissue samples to get a “microscopic” view of the cells, which helps to confirm or rule out the presence of the typical alterations of the esophagus observed in this condition. In fact, the cells of the esophagus of a patient affected by EoE show characteristic alterations that allow for a definitive diagnosis of the condition.
To identify substances that can trigger the symptoms of EoE, patients can take a traditional allergy test such as the prick test or atopy patch test. Both of these tests are based on applying a very tiny amount of the potential allergens on the skin and then observing the skin’s response. There are also a number of blood tests that can confirm an allergic reaction to specific allergens. In all cases, always seek advice from your doctor or specialist on the best tests to carry out and how to interpret the results.
People who suffer from EoE should follow the “elimination diet”. To do this, you start by eliminating allergy-triggering foods that can cause inflammation of the esophagus and lead to the classic symptoms of the disease. These foods can be identified using an allergy test, or you can proceed with the complete elimination of the 6 food groups most frequently associated with symptoms of EoE:
- milk and dairy products
- wheat
- soy
- eggs
- dried fruit and nuts
- shellfish
Depending on how the individual patient responds to the elimination of these foods from his or her diet, after a few weeks, it may be possible to gradually reintroduce some of these food groups in several stages, while monitoring the course of symptoms. All nutritional interventions should be shared with or prescribed by a specialist who will be able to recommend the most suitable and effective dietary regimen for the patient.
The therapy aims to improve the symptoms and reduce the eosinophilic infiltration of gastrointestinal tissue in the esophagus, to achieve the complete remission of the disease. EoE treatment strategies are based on the “3 D’s”: diet, drugs, dilation .
In Italy, a topical, budesonide-based corticosteroid treatment is currently available for managing the condition.
The topical, i.e. local action of the treatment increases the effectiveness of the medication, minimising the potential side-effects.
- Having to eat your meals really carefully and slowly to prevent food from getting stuck in your esophagus?
- Avoiding dried or fibrous foods because they do not go down the esophagus easily?
- Adding lots of sauces or drinking lots of water during meals to make swallowing easier?
- Noticing improvements in your symptoms when you eliminate milk and dairy products, soy, dried fruit and nuts, wheat, eggs and shellfish from your diet?
Do you also suffer from other allergic illnesses, like asthma, atopic dermatitis, allergic rhinitis, or food allergies?
Sources:
- Furuta G.T., Katzka D.A. “Eosinophilic Esophagitis” N Engl J Med. 2015; 373 (17): 1640-1648.
- Gonsalves N.P., Aceves S.S. “Diagnosis and Treatment of Eosinophilic Esophagitis” J Allergy Clin Immunol. 2020; 145 (1): 1-7.
Do you recognise any of these adaptive behaviours?
Speak to a specialist!


